Parents and Families
Thank you for your interest in the AIROPLANE Trial.
If you cannot find the information you are looking for on this page, please feel free to contact us by clicking on this link here
The AIROPLANE trial is aiming to understand how doctors can best support the breathing of premature babies born between 32 and 35 weeks of pregnancy when they need support immediately after birth.
The best possible management of newborns who need breathing support in the delivery room remains a critical area of newborn research. International resuscitation guidelines have changed dramatically over the last 20 years as research has produced more evidence-based practices. Term babies (born after 37 weeks of pregnancy) and extremely preterm babies (born before 28 weeks of pregnancy) have been most widely researched. However, as almost 1 in 10 babies are born premature in Australia, and most of those are born after 32 weeks of pregnancy, it is important to continue to research the best way to care for all preterm infants.
There is currently uncertainty in the care of moderate and late preterm infants (those babies born at 32 to 35 weeks of pregnancy) and a lack of agreement internationally in the optimal starting oxygen concentration when supporting these babies at birth.
Figure 2: Recommended initial oxygen concentrations by gestational age
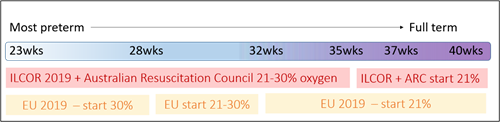
Shown in figure 2, the International Liaison Committee on Resuscitation (ILCOR) guidelines recommend commencing support using 21% oxygen for babies born after 35 weeks of pregnancy, and using 21-30% for babies born earlier. The Australian Resuscitation Council has adopted this recommendation. However, the European Consensus guidelines are a little different. They also recommend using 21% for those babies born after 35 weeks, but they separate less mature infants into three groups; for those born before 28 weeks they recommend starting with 30% oxygen, for those born 28-31 weeks to use 21-30% oxygen, and for those born after 32 weeks to use 21% oxygen (air).
As a result, there is wide variation in what happens in clinical practice locally in Victoria, and around Australia.
We surveyed 20 maternity hospitals in Victoria to find out their standard practice for the oxygen concentration when breathing support is needed at birth for babies born 32-35 weeks of pregnancy. Half of the hospitals told us that support would be commenced using 21% oxygen (air), a quarter of hospitals would start with 30% oxygen, and the remainder recommend using a concentration in the range of 21-30%, leaving the choice of oxygen concentration within this range to the clinician in charge (unpublished data).
We know that both too much and too little oxygen has disadvantages, especially for premature babies. Exposure to too much oxygen generates oxygen free radicals that cause damage to cells and DNA. Too little oxygen does not support the body to function properly. This is why it is important to find out the best possible oxygen concentration to help support a baby's breathing from birth.
The AIROPLANE Trial compares the two different oxygen concentrations that are typically used at birth in hospitals today.
The hospitals taking part in AIROPLANE will be randomly assigned to use an oxygen concentration of either 21% or 30% for a period of approximately 12 months. After this time months, each hospital will then change to using the alternative oxygen concentration for a further ~12 months.
Safety measures have been built into the study design to ensure that every AIROPLANE baby always receives a safe level of oxygen. Should additional care be needed at any time, this will always be provided immediately.
At the end of the trial, we will assess whether either approach leads to babies having less need for later breathing support, oxygen treatment or less time in hospital.
We are automatically enrolling 1,200 infants born between 32 and 35 weeks of pregnancy into the AIROPLANE study.
This study is being led by a group of expert Neonatologists (Newborn Specialists) from the Royal Women’s Hospital in Melbourne. The study is being conducted by doctors at ~20 maternity hospitals around Victoria and NSW. The study is sponsored by the Murdoch Children’s Research Institute, Melbourne Australia.
Babies will be automatically enrolled in the AIROPLANE Study if they are born between 32 and 35 weeks and 6 days of pregnancy and they receive breathing support in the first minutes after birth.
Babies who are born with major complications will not be included.
If a baby is born in a participating hospital and they are eligible to join the study, they will automatically be enrolled in the study.
If a baby has breathing support in the first few minutes of life, doctors attending the birth start that support using the oxygen concentration assigned to their hospital at that time. This will either be 21% oxygen (air) or 30% oxygen. Both are oxygen concentrations already being used today. This research study has been very careful designed with safety measures built in, to ensure that every AIROPLANE baby will always receive a safe level of oxygen. Doctors constantly assess every baby to decide the care they need, and if additional care is needed every baby will always receive that extra support immediately.
After the first 3 minutes of using oxygen at the assigned concentration, the AIROPLANE Trial is completed, and doctors continue to adjust the oxygen concentration each baby needs according to their local guidelines.
Once the baby has been stabilised, and again when the baby is being discharged from hospital, we collect some basic information about the baby’s treatment and progress, gathered from the baby’s medical records.
For any baby whose parents have agreed to be included in the GenV project (a separate research study), we will use some of that information to link these babies’ information together so we can look at longer-term progress of growth and development.
We cannot promise that an individual baby will benefit from this study, as we do not know whether one treatment is preferable to the other, that is precisely what we are trying to find out. However, the results of this study will be used to improve the care of premature babies in the future.
Premature babies can experience complications. However, as all babies in AIROPLANE will receive breathing support and oxygen levels already used in our hospitals today, there is no reason to believe that babies in the AIROPLANE Trial are at any additional risk of complications by taking part.
Yes, there are no restrictions on any other treatments for babies in the AIROPLANE Trial. AIROPLANE babies will receive all the usual newborn treatments, and their day-to-day care will be the same as all other babies who are not in the study. The only difference is how we decide which oxygen level to start support with.
All information will be entered into a secure, confidential, password-protected, purpose-built study database. This information can only be accessed by the research team. No information is ever shared with anyone else.
AIROPLANE has been approved by the Royal Children’s Hospital Human Research Ethics Committee to use a process called waiver of consent. This means that you may not know before your baby is born that the hospital is participating in the study - as doctors are not asked to seek parents’ consent for their baby to take part. This may sound unusual, and indeed it is uncommon for research studies to use a waiver of consent, for very good reasons.
However, in the case of AIROPLANE, the treatments being assessed are part of what we already do. No new treatments are being assessed. AIROPLANE is a safe and thorough way of collecting information about treatments that are already used every day. AIROPLANE has been assessed as being a very low-risk study, and it fulfills the very strict criteria for using waived consent, as laid out by the National Health and Medical Research Council Standards for Ethical Conduct in Human Research.
If you want to know more about what a waiver of consent means, you can read about it here
We asked parents of babies born prematurely - who were cared for in the NICU, and adults who were born preterm themselves about the AIROPLANE Trial. We asked them to help us with the design of AIROPLANE. We particularly wanted to know their thoughts about the use of waived consent. These community representatives were extremely supportive of the trial and felt that waived consent was an appropriate process given that both AIROPLANE treatments are regularly used today, and current parents would not know what treatment their baby had received outside the trial. The parents we asked about waived consent said:
“I think [the study] is incredibly interesting…my opinion is that it would be very low risk, I can’t see any issue with [waived consent]” and “I think [waived consent is] a good idea” and “I don’t have an issue with [waived consent] at all, I think it will be really interesting”
When we asked about how they might feel when they heard that their baby was part of this study after the event, they said:
“I don’t think it would make a big difference to anybody…[if they later found out]. I wouldn’t feel like my child was experimental or anything…” and “I don’t think I would be upset at all”.
These parents are community representatives and are part of the AIROPLANE Trial Steering Committee, using their lived expertise to continue to provide input to the trial processes.
Yes, any baby can be withdrawn from the study. Whilst the waiver of consent means that the trial team do not approach every family to ask whether they would like their baby’s information removed, this will happen at some study sites as per their local guidelines.
Additionally, any family can decide that they do not want their baby’s information included in AIROPLANE and can ask for their data to be removed.
You can ask to speak with the Site Investigator at your hospital, or you can contact the trial team via the contact page on the website. You do not need to give a reason why you would like your baby’s information to be removed from the project and doing so will not affect any of the care your baby receives.
This study is being conducted by the AIROPLANE trial team led by Associate Professor Louise Owen, along with a collaborative group of expert neonatal clinical researchers from the Royals Women’s Hospital in Melbourne. The trial is supported by the Murdoch Children’s Research institute and the Melbourne Children’s Trial Centre.
The research is funded by the University of Melbourne and the Centre of Research Excellence in Newborn Medicine.
If you have questions or any concerns regarding the AIROPLANE trial please talk with the medical team at your hospital, or contact the trial management team through the contact page on this website